Medical respite care helps Michigan’s most vulnerable recuperate after hospitalization
A handful of Michigan facilities offer daily wound care, help filling and taking prescriptions, or support with substance use disorder treatment for those in need.

This article is part of State of Health, a series about how Michigan communities are rising to address health challenges. It is made possible with funding from the Michigan Health Endowment Fund.
Many Michiganders leave the hospital still needing more care than is available or affordable for them. They may need daily wound care, help filling and taking prescriptions, or support with substance use disorder (SUD) treatment. While Medicaid, Medicare, and private insurance may cover some post-acute hospital care, many Michiganders cannot find the support they need to fully recover.
However, a handful of Michigan facilities offer the support these individuals need, known as medical respite. The National Institute for Medical Respite Care (NIMRC) describes medical respite, also known as recuperative care, as “short-term, residential care that provides a place to rest, recover, and heal to people experiencing homelessness who have been discharged from hospital-level care.” In addition, medical respite care connects individuals with other supportive services, such as housing, employment opportunities, and mental health resources.
The Salvation Army operates two medical respite facilities in Michigan, Detroit Medical Respite and Southeast Michigan Medical Respite in Monroe. Michigan’s other two medical respite facilities are HOPE Recuperative Care Center in Pontiac and the Shelter Association of Washtenaw County’s Recuperative Care Program in Ann Arbor. According to Jamie Winkler, executive director of the Salvation Army Great Lakes Harbor Light System, the Salvation Army hopes to expand medical respite services into other areas of the state.

“The last that I heard, there’s about 85 medical respite programs across the country. So, in many respects, medical respite is still a little bit of a novelty,” Winkler says. “The idea behind medical respite is: what does a hospital do when someone’s healthy enough to be discharged from a hospital, but they’re homeless or they could become homeless? How does the hospital safely discharge someone?”
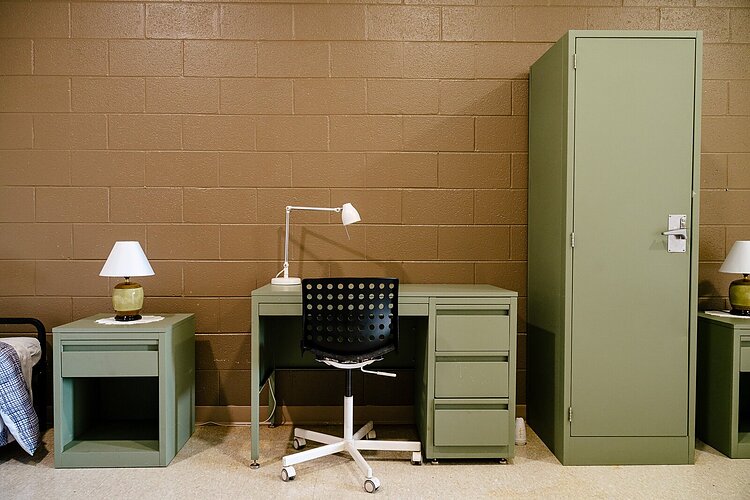
Medical respite sites offer a safe, clean, 24-hour healing environment for unhoused individuals in need of post-hospitalization care. After coordinating discharge with the hospital, they help patients manage medications, wound care, and follow-up visits with health care providers. They ensure patients have food and behavioral health supports. Case managers can help individuals plan for improved lives after they leave.

“Medicaid does not necessarily recognize medical respite and because of that, programs have needed to be a little creative in how they get their funding to make it a reality,” Winkler says. “Some use foundation money, and there are some [billing] codes for homeless services that [non-governmental organizations, or NGOs] can draw down on. Other NGOs use some of their administrative monies to help this population. It’s a little bit challenging to get [a medical respite facility] going and for people to understand the value.”
At-risk demographics
The need for post-hospital care crosses all demographics and income levels. However, being an older adult, living alone, having income challenges, or being unhoused raise the risks for poor health outcomes and hospital readmissions.

“Sometimes it’s not even income-related,” says Laura Appel, executive vice president government relations and public policy for the Michigan Health and Hospital Association. “But certainly, people with fewer monetary resources, people without adequate housing, or people with no home at all are most at risk for having poorer outcomes if they need post-acute care.”
For older adults, poor health is a major cause of homelessness.
“Right now, I’m in really good health. I don’t take any medicine. But if I have a stroke, that could put my family in a bit of a tailspin,” Winkler says. “That’s what happens to so many Americans. Some kind of health care issue caused them to not be able to maintain their mortgage or their rent.”
Winkler recently worked with a woman who had been a professional, had a master’s degree, and was living in her car. She went three days without food before asking the Salvation Army for help. Another individual Winkler worked with is living in his car and needs a hip replacement. Before the hospital will allow the procedure to be done, he must have stable housing. In addition, people who are medically frail and living with homelessness often fear staying in a shelter.
“I know this person who has a colostomy bag and other health care conditions going on. He didn’t want to go to a shelter because of this bag. It leaks sometimes and he’s been beaten up because of it,” Winkler says. “So, our program provides prompt access to care. We give people dignity, love, and respect. And we give them an environment where a home health nurse can come, where we can make sure that they follow through with their discharge plan from the hospital and with their medication compliance.”
Substance use disorders increase risks after hospitalization
Another population that can be harshly impacted by lack of post-hospitalization care is those living with SUD.

“If there’s a medical complication that resulted in their hospitalization, then it’s really critical that they stay engaged with any type of treatment or intervention service,” says Greg Toutant, executive director of Great Lakes Recovery Centers. “The risk for relapse is so much higher because of the pressures they’re under in terms of managing issues medically that led them to hospitalization. Also, they’re going to be struggling with issues on payment for hospitalization, insurance coverages, housing, job issues, you name it. All of those social determinants of health get exacerbated after a hospitalization.”
While the Upper Peninsula region that Great Lakes Recovery serves does not have a dedicated medical respite facility, Toutant says its peer recovery coaches and care coordinators from Upper Peninsula Health Plan, a Medicaid and Medicare advantage health coverage provider, do a good job of checking in with patients living with SUD after they are discharged from the hospital and connecting them to supports.
“Peers are really good in their ability to navigate the systems around them, especially for public assistance, insurance-related issues, and housing,” Toutant says. “It could be a host of barriers that a client might face after coming out of a hospitalization. They need more intensive wraparound support. We know recovery housing could also be a strong need that people may have, especially if they’re convalescing from something.”
The post-hospitalization period is also a good time to introduce treatment to those who are not already enrolled in a recovery program.
“It’s a vulnerable time when they leave [the hospital] and a time for introspection,” Toutant says. “If we can break them of whatever they’re struggling with, as far as an addiction or an abuse of a certain substance, then it’s a great time to … link them with services.”
The bottom line
People experiencing homelessness stay in the hospital longer than housed patients, resulting in substantially higher costs. When these same people cannot adequately care for themselves after a hospitalization, they often are readmitted. Providing medical respite reduces readmissions as well as the associated costs for health care systems and payors like Medicaid and Medicare. Winkler says that on average, people experiencing homelessness stay in the hospital for about two and a half days longer than those who have stable housing.
“Back in 2016, when we were coming up with our model, the state’s average for hospital care was about $2,100 a day,” Winkler says. “If you take that $2,100 a day and you multiply that by two and a half days, you know the [medical respite programs] provide a cost savings that promotes health.”
The Kaiser Family Foundation reported Michigan’s average 2020 “Hospital Adjusted Expenses per Inpatient Day” at $2,681. Detroit Medical Respite costs run $175 a day, making an average 30-day stay there cheaper than a two-day stay at a hospital.
In Michigan and across the nation, people experiencing homelessness, those living alone, and others who do not meet criteria for Medicaid income caps or qualified Medicare services need more access to medical respite care. Without it, the pain and suffering that they experience devastates their lives and increases costs to health care systems.
“There’s probably more understanding about how what looks like an additional expense saves costs in terms of readmissions and human suffering,” Appel says. “I think we’re moving in the right direction, but we probably need to be doing more of it and creating more access for it.”
Estelle Slootmaker is a working writer focusing on journalism, book editing, communications, poetry, and children’s books. You can contact her at Estelle.Slootmaker@gmail.com or www.constellations.biz.
Salvation Army photos by Nick Hagen. All other photos courtesy of the subjects.





